By Ann-Lena Farrington Wigan and Leigh Hospice, Inpatient Unit
Pressure ulcers are sometimes known as pressure sores or bed sores.
Pressure ulcers are difficult to heal, leave the individual prone to infection and are painful. Additionally, they are usually preventable – the only exception is for people with certain conditions.
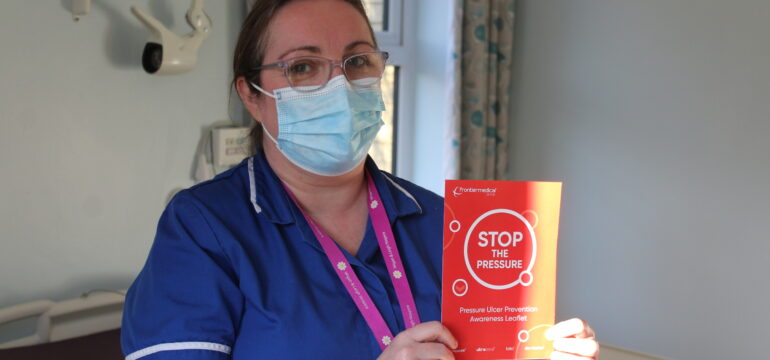
Over the last 12 months we have been very active at the hospice in educating staff on pressure ulcer prevention. This has included attending regular training, updating our pressure ulcer policy and ensuring equipment, including specialist mattresses are well maintained. We often speak to the tissue viability nurses at Wigan, Wrightington and Leigh NHS Trust and attend regular training.
What is a pressure ulcer?
They are skin damage which usually occur on a bony part of the body so often develop on heels, elbows or buttocks. They develop in places where pressure is applied or where friction has occurred.
What do they look like?
The first sign will be a redness that looks like the redness you get when you’ve been leaning on something – but this redness doesn’t go away. You should also look out for numbness, pain or breaks in the skin.
That redness would be what is called a Category One pressure ulcer. There are a number of stages ranging from this redness which, if left unmanaged to the extreme, can become a deep wound.
What causes them?
They are usually caused when someone has reduced mobility, is ill or is on certain medications.
How are they prevented by professionals?
We can prevent pressure ulcers by using specialist mattresses and turning people regularly but also by educating people on pressure ulcers and addressing mobility issues.
Everyone who comes into hospice is assessed. Our patients are high risk as they may have reduced their activity so we always check the skin and keep it clean and dry.
How can I prevent pressure ulcers myself?
The best way to do this is to change your position regularly. You should also maintain your skin – this means keeping it dry and clean and using creams when needed.
Are certain people more prone to getting pressure ulcers?
People who obese or malnourished may be more likely to develop a pressure ulcer.
People living with breathing conditions, poor circulation, approaching end of life, those who are on long-term steroids, have dementia or are paraplegics are also more at risk of developing a pressure ulcer.
I think I have a pressure ulcer. What should I do?
Report any concerns to your GP or district nurse.
Where can I get more information?
There are good resources on the NHS website. The Stop the Pressure Campaign also has a website.